Tennis elbow (Epicondylitis humeri radialis)
explained by Philipp R. Heuberer, MD, shoulder, elbow, knee specialist
I know from my practice as a shoulder, elbow and knee specialist:
Lateral epicondylitis or tennis elbow is one of the most common problems in the forearm area – more precisely: on the outer side of the elbow. Learn all about the triggers and symptoms as well as the different methods of tennis elbow treatment.
What is tennis elbow?
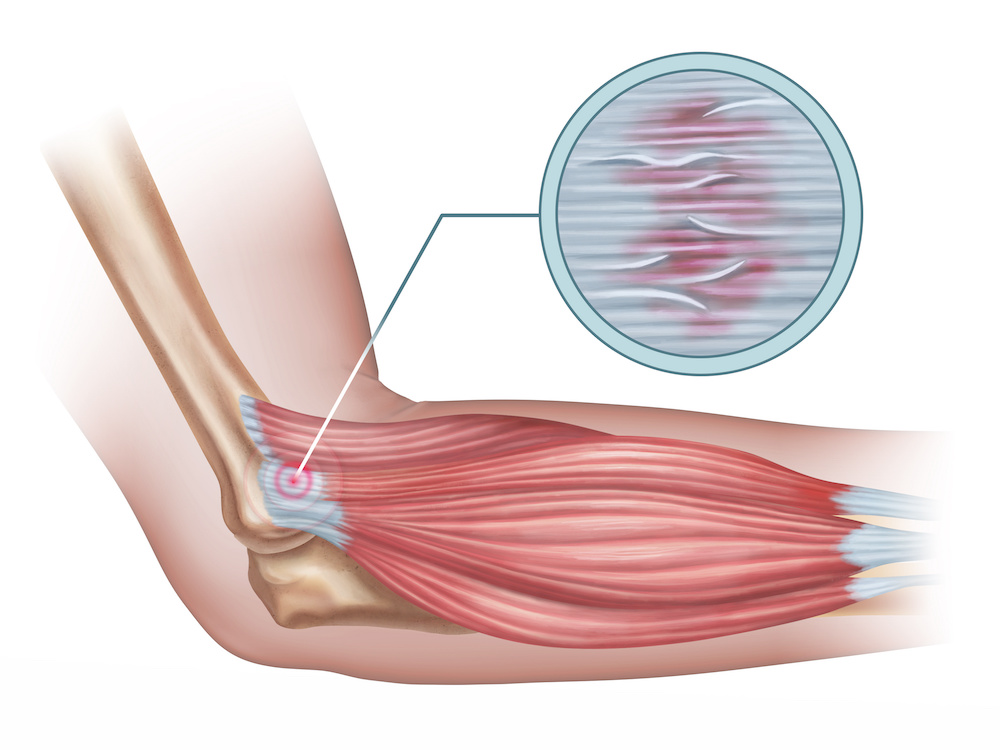
Lateral epicondylitis, also known as tennis elbow ia a tendon disease of the extensor muscles of the forearm caused by chronic overuse.
In tennis elbow, the tendons at the insertion on the outside of the elbow (lateral epicondyle) are irritated because of overuse, which is usually accompanied by severe pain. Mostly affected are the tendon insertions of the muscles responsible for the extension of fingers and the movement of the wrist.
By the way: If the irritation occurs on the inside of the elbow (medial epicondyle), it is not called tennis elbow, but golfer’s elbow or ulnar epicondylitis.
In the course of the diseases, this irritation can turn into a mostly irreversible degeneration of the tendons.
How do the symptoms of a tennis elbow manifest?
Typical symptoms of tennis elbow are pain on the outside of the elbow, but in the case of golfer’s elbow, the pain is felt on the inside of the elbow. Initially, there is an unpleasant feeling of pressure in the joint of the elbow, which becomes increasingly painful.
When pressure is applied to the bony prominence, as well as when stress is applied to the irritated tendons, the pain is felt to be more intense.
If initially mainly the elbow is affected, the pain can radiate over time into the forearm to the wrist and fingers. Additionally, numbness in the arm or tingling in the fingers may occur.
It is not uncommon for tennis elbow to be accompanied by weakness in the wrist. In addition to the great pain, this can cause other problems in everyday life, such as when cups, pens or other objects can no longer be held or used.
What are the causes of tennis elbow?
In the vast majority of cases, tendon irritation is caused by overloading or overuse of the forearm muscles – and in particular the muscles responsible for wrist movements and finger extension. Triggers are mainly one-sided or excessive overuse.
Tennis elbow, as the name suggests, can be caused by playing sports such as golf, squash, baseball or tennis.
However, golfers and tennis players are not the only ones at risk of tennis elbow. On the contrary, even a uniform or repetitive movements in everyday life and especially in professional life can cause an epicondylitis.
Prolonged screwing, sawing, hammering, ironing, typing, or similar monotonous performances are common causes of tennis elbow. Office workers are therefore just as affected as physically working people and hobby athletes.
Incorrect posture or unfavorable lying and sleeping positions can also lead to the occurrence of tennis elbow in individual cases.
Which people are particularly susceptible to tennis elbow?
A tennis elbow often occurs between the ages of 30 and 55. People with weakened and shortened arm and especially forearm muscles are considered particularly susceptible.
How is a tennis elbow diagnosed?
The diagnosis of tennis elbow comes from a thorough examination and an x-ray, which is used to rule out bony causes. Magnetic resonance imaging can then be used to visualize the tendon damage.
What can you do against tennis elbow?
With the right therapy, very good success can be achieved with conservative treatment.
The popular belief that the best option for relief is rest and ice of the affected arm can no longer be maintained.
A successful treatment is composed of three pillars, basically helping the body to heal itself. The full-blown tennis elbow or golfer’s elbow is usually a chronic degenerative tendonitis that heals very, very slowly on its own, usually over years, due to the poor blood supply to the tissue.
The first condition is that the chronic inflammatory situation must be converted back to an acute one in order to create a more favorable healing environment. I use electrolysis for this purpose, whereby degenerative tendon tissue is denatured under ultrasound-guidance. The injection of the body’s own growth factors (PRP, blood plasma) is then used to promote healing.
Another pillar is extracorporeal shock wave therapy, whereby pressure waves stimulate stem cells and growth factors in the bone, which promote tendon healing, which always starts from the bone. The alternation of these therapeutic methods is done according to the principle: “Fertilize the earth and water the lawn”.
The third and, in the long run, most important pillar is proper training with exercises precisely tailored to the complaints. It is known from numerous studies that forms of eccentric training, which is a negative loading of the muscles, induce and influence the proper alignment, reformation and shaping of tendon fibers.
Cortisone injections, however, should be avoided. Indeed, numerous studies proved that these injections have only a short-term effect, but damage the tissue in the longer term.
Only if the symptoms do not improve despite intensive therapy for at least 3 months, surgical intervention may be necessary.
However, with the above therapy regimen I developed, I have not had to operate on a single elbow due to tennis elbow or golfer’s elbow in recent years.
When does a tennis elbow require surgery?
In most cases, conservative treatment already leads to success. If, despite intensive therapy, there is still no improvement in sight after 3 months, or better still after 6 months, surgical intervention may be necessary.
Through this procedure, where the degenerative tendon tissue is removed and the tendon attachment to the bone is reattached, the pain can be very effectively relieved and the tendon can usually be restored to regeneration. However, most patients are left with minimal loss of strength. Sports and occupational activities may remain restricted for longer due to a rehabilitation period of 3 to 6 months.
The procedure can be performed arthroscopically or openly, but diagnostic arthroscopy of the elbow should always be performed beforehand to rule out posterolateral rotational instability.
After the operation, the forearm should be rested for 2 weeks and then the forearm muscles should be stretched and built up again as part of remedial gymnastics. If posterolateral rotational instability is present, change to another surgical procedure (see posterolateral rotational instability).
How long does the treatment of tennis elbow take?
It is difficult to give a straight answer to this question. Depending on how far the inflammation has already progressed and which treatment method is relied on, the treatment and the associated healing of tennis elbow can take up to least several months.
What happens if tennis elbow is not treated?
Many people neglect the initial symptoms of tennis elbow, such as mild pain in the lateral aspect of the elbow or minor painful movement restrictions, and treat them with medications such as painkillers, creams and ointments, or apply a commercially available epicondylitis brace.
However, if you experience pain in your elbow, you should see a doctor immediately so that a diagnosis can be made quickly. Because: untreated symptoms can develop into a chronic problem that accompanies and affects those affected for a long time.
If no action is taken, it can usually take up to 5 years for the body to heal the tendon on its own. However, during this time there is usually severe pain that does not allow manual activity for a long time.
What is affected?
The biceps is a two-headed muscle that connects the shoulder to the elbow and performs flexion at the elbow. Coming from the shoulder with two tendons, the biceps joins at the elbow to form a tendon that attaches extensively to the radius.
This tendon attachment can become inflamed (tendinitis), which can lead to a painful partial rupture and finally to a complete rupture.
Biceps tendinitis causes pain in the elbow due to inflammation. Partial rupture leads to weakness and dysfunction of the muscle via inflammation. The complete tear is a severe soft tissue trauma with copious bleeding and swelling.
read more...
How is it determined?
The diagnosis of complete biceps tendon rupture is clinically apparent. An ultrasound or MRI confirms the diagnosis and shows how far the tendon has retracted into the upper arm. Tendinitis or partial rupture can only be confirmed by MRI or ultrasonography.
How to treat the discomfort?
A rupture should be operated as soon as possible, as the tendon can retract severely, and extensive reconstruction with donor tissue may then be necessary. Tendinitis as well as partial rupture can be treated conservatively in the first instance. Eccentric training, focused shock wave therapy, and ultrasound-guided injections with PRP are promising.
In case of failure of conservative therapy or a complete tear, the tendon stump is refreshed and anchored back into the radius during surgery. In my preferred, but not simple, technique, the stump of the tendon is anchored in the depth of the elbow with a metal button in a blind hole in the radius, sparing important nerves and vessels. This surgical technique with the most stable fixation means that no immobilization is necessary postoperatively and immediate movement is possible. Isometric strength training is not allowed until after 6 weeks, and a return to manual activity or sports is not allowed until after 12 weeks.
...less text
What is affected?
In elbow stiffness, the soft tissues around the elbow thicken and stick together. Scar strands form in the joint, restricting movement. Ossifications can form as well.
The importance of elbow function is not immediately obvious, but is extremely limiting when lost, as basic needs such as bringing the hand to the head to eat, drink, blow the nose, put on glasses, and more depend on it.
Inability to bend or extend the elbow or to perform a twisting movement is called elbow stiffness or restricted movement.
read more...
How is it determined?
Diagnosis is made after clinical examination and by X-ray. The extent of new bone formations is best assessed on computed tomography; MRI shows mainly soft tissue thickening.
It is important to first determine why the elbow stiffness occurred, since sometimes a ligament instability can be behind it, which then also needs to be addressed.
How to treat the discomfort?
In principle, the treatment is conservative. Especially a pure soft tissue stiffness with thickening of joint capsule, tendons and ligaments can be treated very well with physiotherapy and ultrasound-targeted hydrodilatation. This is done analogously to the shoulder, inflating the joint with a mixture of local anesthetic, cortisone, and lots of sodium chloride solution.
Recalcitrant soft tissue stiffness or elbow stiffness caused by bony causes then require surgical intervention by means of arthroscopy, capsular mobilization, removal of bony obstructions, and possibly nerve mobilization.
It is important to mobilize the elbow immediately and consistently after surgery, ideally under a pain block in which the arm nerve plexus is switched off.
...less text
What is affected?
Osteoarthritis of the elbow is less common than in other joints due to the less severe stress and also causes less pain. Predominant is the restriction of movement, which is the main problem.
Causes of elbow osteoarthritis are fractures caused by direct trauma, but also slight changes in the mechanics of the elbow, causing post-traumatic osteoarthritis, although only parts of the joint may be affected. Normal elbow joint wear is rare, but can occur with certain manual activities, such as work with a sledgehammer.
Repeated microtrauma, such as boxing or even after fractures, can cause loose joint bodies to form, leading to entrapment symptoms.
read more...
How is it determined?
An X-ray shows the wear and also already loose bodies in the elbow. MRI can be used to precisely localize the cartilage lesions, and CT can then be used to localize the free joint bodies.
How to treat the discomfort?
Osteoarthritis, especially in the elbow joint, can be successfully treated conservatively for a very long time. Exercise therapy, manual joint distraction, and especially then regenerative measures such as ultrasound-guided injections with PRP, stem cell concentrates if necessary, and hyaluronic acid can regenerate the joint environment and reduce friction so that the inflammatory response is suppressed.
If conservative therapy fails or if there are signs of entrapment due to free joint bodies, surgical intervention by arthroscopy is recommended to remove the painful synovia, loose bodies and sharp-edged osteophytes. After such a procedure, the elbow should be moved immediately and the pain-free result should last at least 5-7 years.
Only in rare cases of pronounced osteoarthritis surface or joint replacement is indicated.
...less text
What is affected?
Chronic overuse, repeated microtrauma or even major trauma can lead to injuries of the lateral ligamentous apparatus at the elbow and thus to instability. Often, this pain can be misinterpreted as medial or lateral epicondylitis (tennis or golfer’s elbow) and accordingly treated conservatively for a long time without success.
First and foremost, throwing and impact sports, as well as recurrent overuse and microtrauma to the elbow, pose the risk of permanent instability, in addition to major injuries such as elbow dislocation. In particular, the primary suspected diagnosis of epicondylitis and its treatment with cortisone injections can contribute to further injury to the collateral ligament apparatus.
read more...
How is it determined?
The diagnosis of elbow instability or collateral ligament injury is often difficult. The patient typically does not come to the physician with a complaint of instability, but reports the nonspecific symptom of “pain.” Clinical examination of lateral ligament instability is performed by stress testing of the lateral ligamentous apparatus. On the inner side, instability can usually be diagnosed very well. However, the more common posterolateral rotational instability on the outside can often be inadequately detected. The problem is that due to the muscular bias, it is hardly meaningful in the awake patient. Only during anesthesia or under arthroscopic control does a provocation test reveal the true instability. Because in posterolateral rotational instability the anatomic unit of radius and ulna rotates out of the joint to the humerus due to instability of the radial (external) collateral ligament complex, this rotational motion is often announced as the mechanism of trauma.
An MRI scan is also a very sensitive exam to detect a collateral ligament injury. Unfortunately, the findings are often misinterpreted as inflammation, and the severity of the instability cannot be determined either, since MRI is a static examination. However, concomitant pathologies such as loose bodies, cartilage damage, subluxation positions of the joint, etc. can be visualized very well.
Ultimately, diagnostic elbow arthroscopy is the last resort to reliably detect posterolateral rotational instability and perform reconstruction of the insufficient ligaments with autologous tendons to restore joint stability.
How to treat the discomfort?
Treatment is exclusively surgical, reconstructing the torn ligament. This is done with a combined procedure of arthroscopic and open approach. After the instability is identified during elbow arthroscopy, a piece of the triceps tendon is openly harvested and then woven between the humerus and ulna as a ligament replacement. Postoperatively, a splint must be worn for 6 weeks, with movements already allowed during the last 2 weeks. After that, strengthening exercises can be done. Full loading is possible again after 3 months. The surgery has a success rate of over 90%, but only if performed by a specialist, as it is an extremely complex procedure.
...less text